Navigating increasingly complex clinical audits
Published:
December 17, 2025
Clinical audits are becoming increasingly complex, demanding, and time-consuming. What should be a shared focus on patient care and payment accuracy often becomes a source of friction—driven by inconsistent criteria, documentation challenges, and labor-intensive review processes.
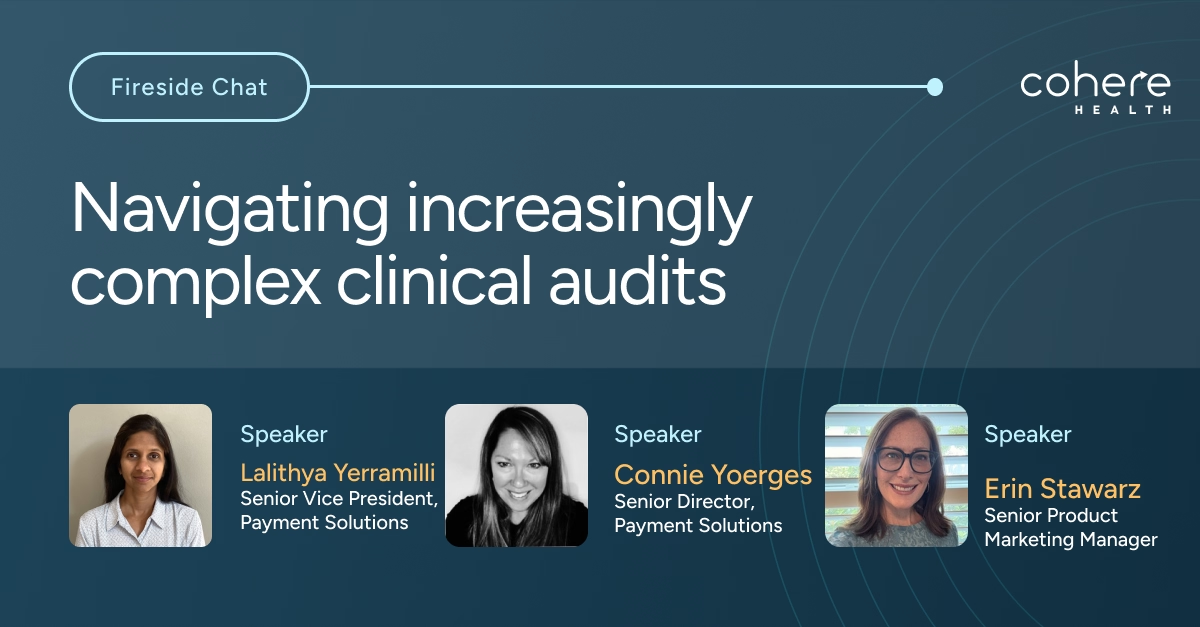
In this fireside chat, payment integrity experts explore the realities of modern clinical audits. Listen in to hear the challenges faced by PI teams, dive deeper into sepsis audits as a high-stakes example of clinical and operational complexity—and walk away with actionable insights your teams can apply today.
Watch the conversation to learn:
- Why clinical audits are so challenging: From lengthy medical records to complex coding and policy interpretation, auditors face mounting pressure to deliver accurate decisions quickly and consistently.
- Why sepsis pushes audits to the limit: Evolving definitions (Sepsis-2 vs. Sepsis-3, SOFA, qSOFA), inconsistent documentation, and differing payer policies create downstream impacts on reviews, appeals, and provider trust.
- Where payer–provider gaps emerge: How misalignment between documentation and interpretation leads to delays, denials, and administrative burden on both sides.
- How technology can help bridge the divide: How precision, transparent AI—paired with human clinical expertise—can support faster reviews, clearer decisioning, and more transparent communication.
Learn how health plans are rethinking clinical audits—not just as a payment integrity challenge, but as an opportunity to improve collaboration, accuracy, and trust across the healthcare ecosystem.




