How Cohere Connect™ works
Partner with technology and UM experts
Cohere Connect was developed in partnership with clinical prior authorization experts to be configurable and support changing policies and frequently updated member requirements.

AI-Powered prior authorization automation
Offerings:
Flexible models and meaningful insights to insource high-value audits
Offerings:
Ready to update your clinical and coding decision-making?
By Stakeholder
Empowering stakeholders with AI-driven solutions for prior authorization and payment integrity.
Offerings:
Flexible, specialty-specific solutions and actionable insights for high-value care management.
Ready to update your clinical and coding decision-making?
A scalable interoperability solution aligned with CMS-0057-F to power your enterprise prior auth strategy.
A scalable interoperability solution aligned with CMS-0057-F to power your enterprise prior auth strategy.
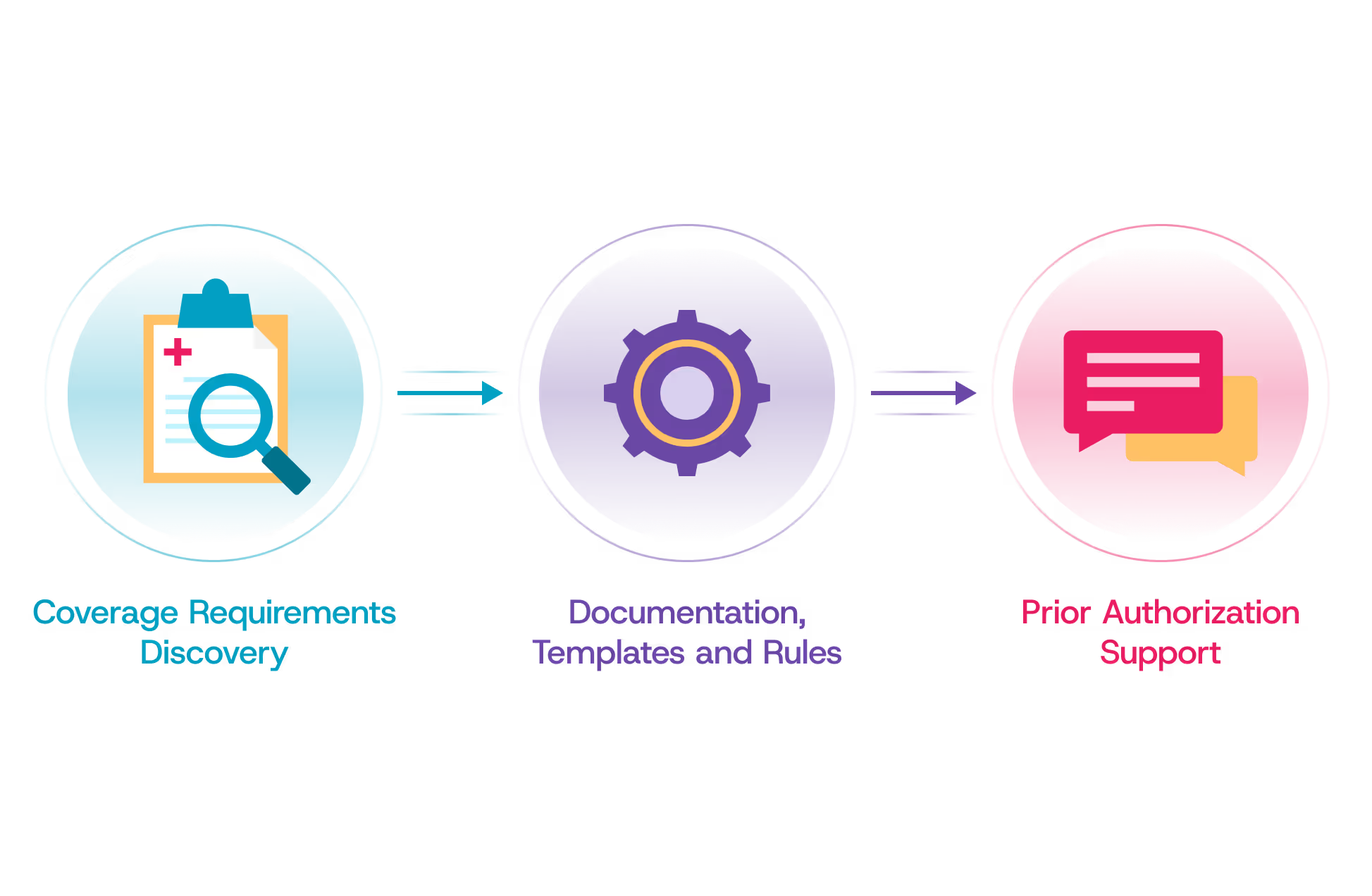
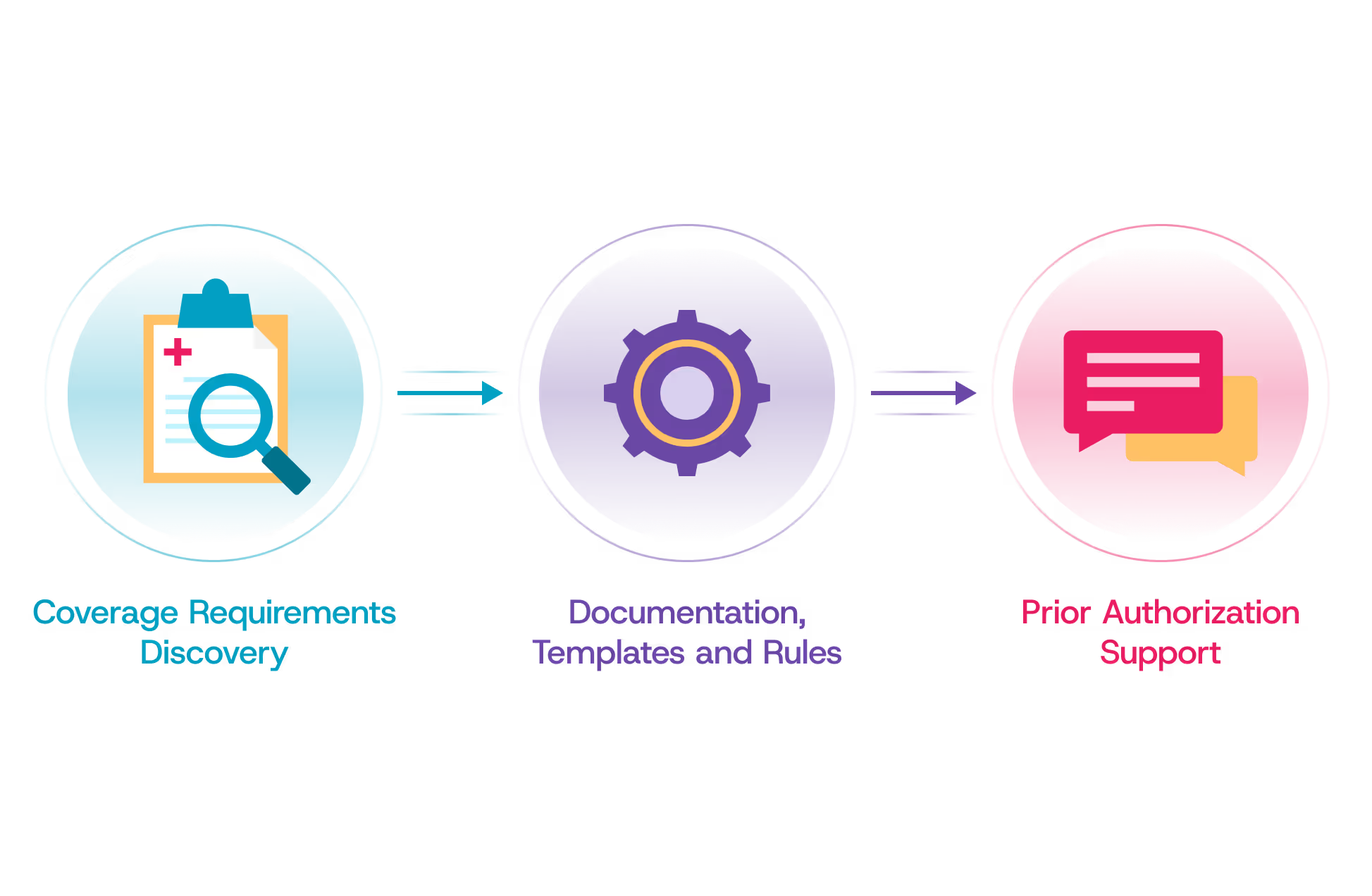
How Cohere Connect™ works
Cohere Connect was developed in partnership with clinical prior authorization experts to be configurable and support changing policies and frequently updated member requirements.

Give providers the exact documentation requirements, configurable by procedure, diagnosis, place of service, and provider type.

Give providers a single front door for routing prior authorization requests.

Address a broad range of policies, including CMS, industry guidelines, and your custom medical policies.
Benefits
Cohere Health streamlines the prior authorization process, making it efficient and effective. With our platform, health plans can leverage automation to enhance clinical decision-making.

Drive interoperability across your PA workflow and reduce provider burden.

One vendor for all the prior authorization FHIR APIs to support CMS-0057-F.

Ensure a sound DTR workflow with expert policy digitization services available.
Overview
Our production-ready APIs are actively serving health plans nationwide. We not only meet HL7® Da Vinci™ Implementation Guide standards and support SMART® on FHIR® applications—we enhance them with essential capabilities that create truly efficient prior authorization workflows.
API
Purpose

Coverage Requirements Discovery (CRD)
Instantly verify if prior authorization is required and confirm service coverage.

Documentation Templates and Rules (DTR)
Intelligently gather and submit all required documentation for the request.

Prior Authorization Support (PAS)
Submit authorization requests and learn the outcome

Give providers support to deliver the right information up front and adhere to rules with Cohere’s API-based process prompts

Improve the quality of medical necessity reviews with policy digitization services performed by interoperability and prior auth experts

Configure clinical documentation requirements based on procedure, diagnosis, site of service, and more

Give providers a single front door for compliant, API-based auth submissions–regardless of the vendor managing authorizations
Validated impact
Real results from payers and providers.
93%
provider satisfaction rating
4000+
digital policies supported
15M+
authorizations leveraging APIs




While others scramble to adapt, our API-ready solution is already processing millions of authorizations.




While others scramble to adapt, our API-ready solution is already processing millions of authorizations.
Explore common questions about Cohere’s fully delegated utilization management services.
CMS-0057-F Applies to Medicare Advantage, Medicaid, and CHIP Fee-for-Service as well as Managed Care and Qualified Health Plans (QHPs) in the Federally Facilitated Exchange. It does not apply to Commercial plans, however some states are pushing forward with similar mandates that apply beyond the CMS prior auth rule’s scope to include Commercial lines of business.
No, Cohere Connect is a standalone offering from Cohere that does not require the purchase of in-house automation or delegated prior auth solutions. Cohere Connect can empower health plans to quickly achieve compliance with the FHIR API workflow requirements of CMS-0057-F.
Yes, Cohere Connect can be configured to act as the single front door for your providers’ prior auth submissions.
In response to CMS-0057-F, the National Standards Group will not take HIPAA Administrative Simplification enforcement action against HIPAA covered entities that choose not to use the X12 278 standard as part of an electronic FHIR prior authorization process.