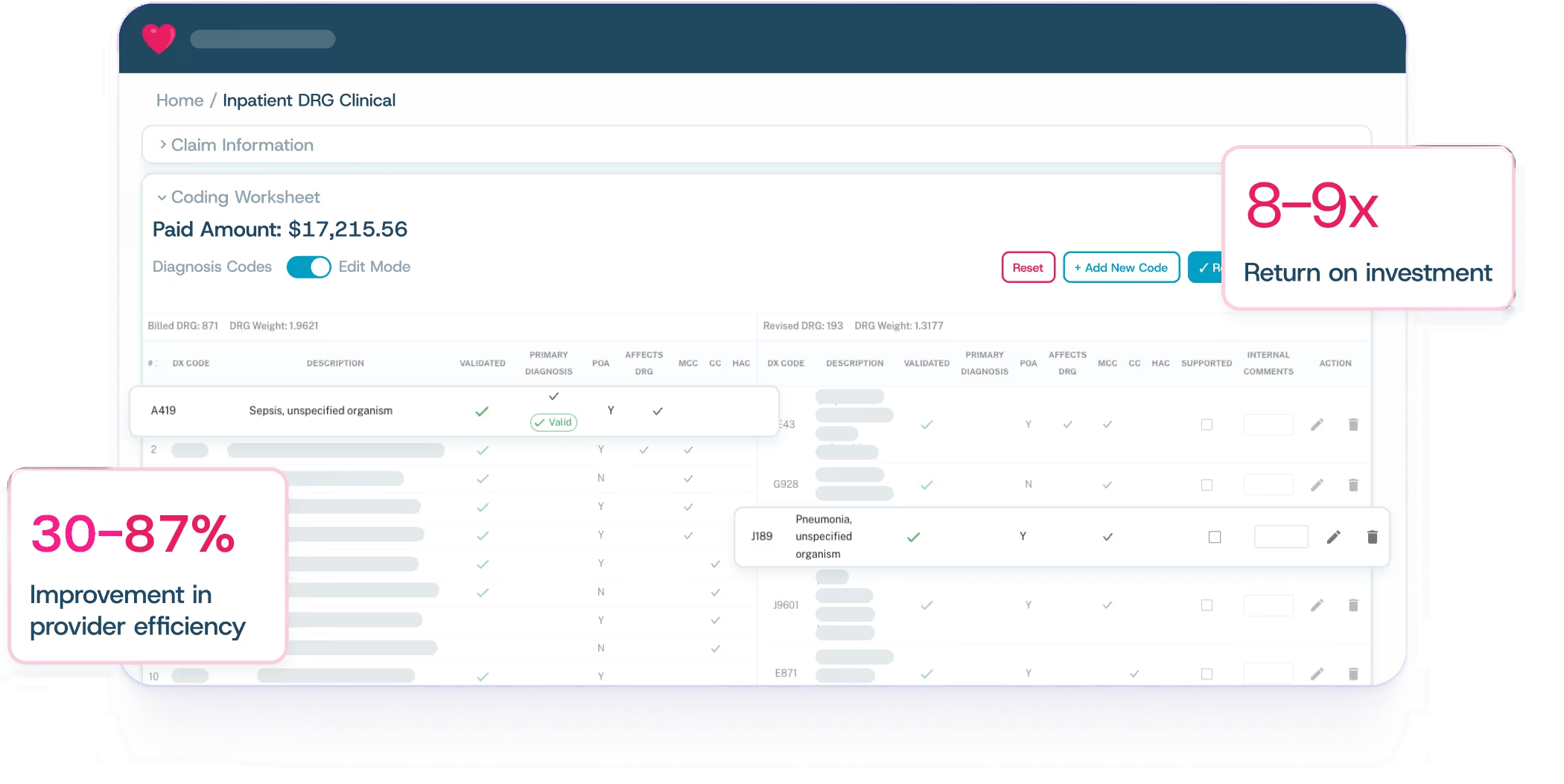
Reduce inaccurate payments and scale in-house PI operations with Cohere Validate™.
Strategically enhance your internal team’s capabilities to drive better outcomes.
Intelligent selection, automated edits, and accelerated, clinically accurate workflows to empower your in-house team across prospective and retrospective reviews
Intelligent selection, automated edits, and accelerated, clinically accurate workflows to empower your in-house team across prospective and retrospective reviews
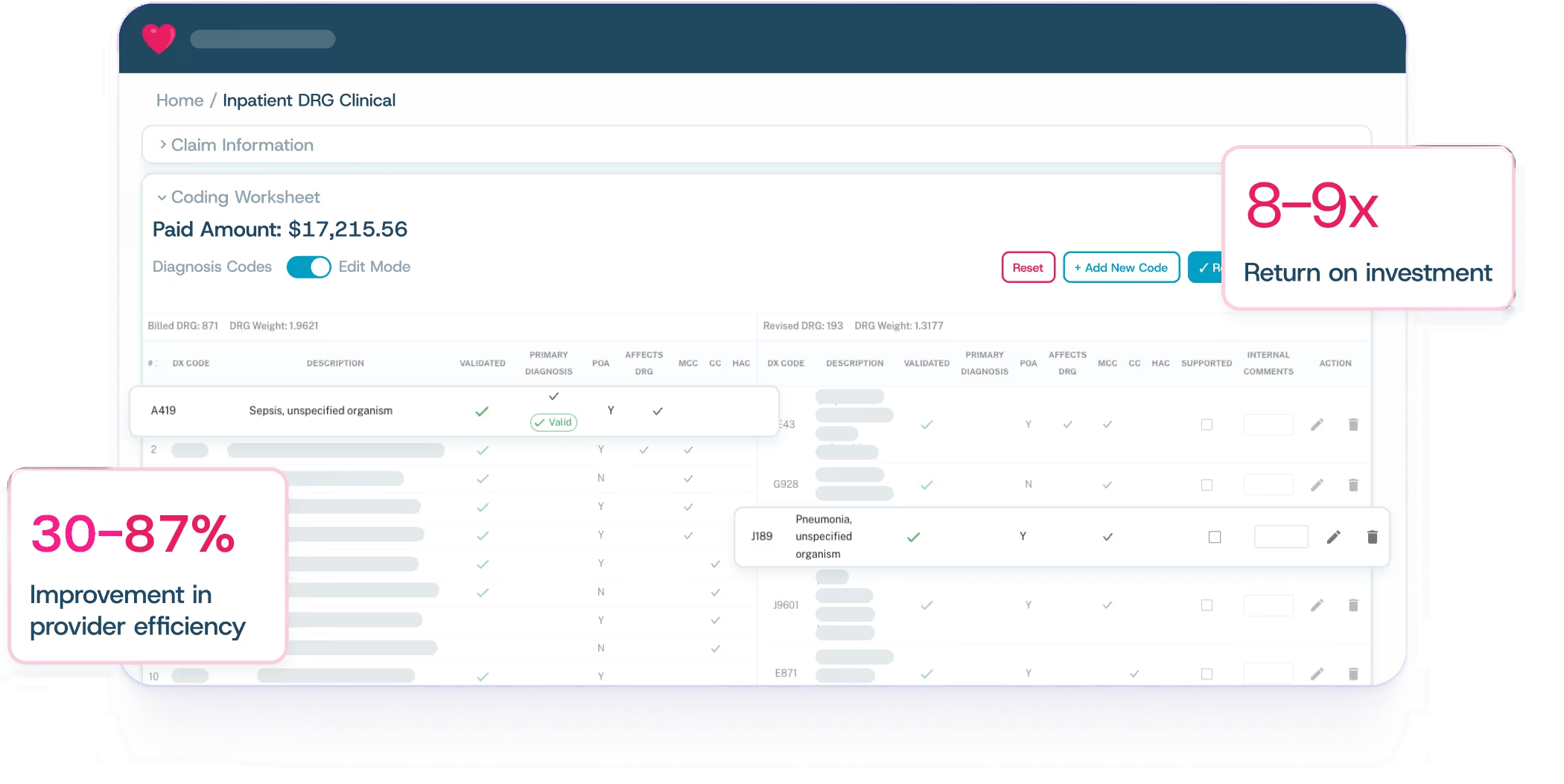
See how Cohere Validate's transparent AI can help your team perform complex clinical and coding validation with unprecedented efficiency and accuracy.

See how Cohere Validate's transparent AI can help your team perform complex clinical and coding validation with unprecedented efficiency and accuracy.
