How Cohere Health is redefining payment integrity with AI
Published:
September 19, 2025

Health plans often rely on a patchwork of outsourced payment integrity (PI) vendors to ensure payment accuracy. While these vendors deliver savings, their contingency fees are high, their methods are opaque, and their fragmented audit approaches often increase provider abrasion. This model mirrors the legacy delegated approach on the UM side—with limited transparency and strained payer-provider relationships.
Cohere is charting a new path. With Cohere ValidateTM and our broader PI Suite, we’re bringing the same precision AI and configurable model that redefined UM into the payment integrity space. Our PI suite gives health plans the option to insource, augment, or delegate PI operations in a way that drives accuracy, transparency, and trust.
Why payment integrity needs to change
PI is a mature and crowded market, dominated by stacked vendors and opaque reviews and audits. The challenges are clear:
- Vendor sprawl and dependency: Health plans often manage multiple PI vendors with as high as 30% contingency fees.
- Opaque operations: Traditional PI vendors rarely share root cause insights, limiting health plans’ ability to intervene upstream, fix systemic issues, and strengthen provider relationships.
- Provider abrasion: Fragmented PI operations lead to duplicate record requests, delayed payments, and strained relationships with provider networks.
- AI on both sides: Providers increasingly use AI to auto-generate appeal letters, escalating the arms race between payer cost containment and provider counter-audits.
At the same time, industry momentum is shifting. Health plans are showing growing interest in pre-pay solutions. The “shift left” approach to earlier intervention promises faster, more accurate payments and stronger provider trust, but it requires advanced AI-driven technology to make it possible.
Enter Cohere Validate
Cohere Validate is designed to meet these challenges head-on. Much like in UM, our payment integrity solutions are powered by precision AI trained specifically on reimbursement methodologies. By combining automation, transparency, and clinical expertise, Cohere Validate modernizes how health plans approach the most complex audits and reviews.
Key capabilities include:
- Comprehensive coverage: Inpatient, outpatient, and professional claims
- Seamless UM-to-PI integration: Leverage Cohere’s UM data to refine case selections and gain a unique advantage
- Automated clinical and coding validation: With human safeguards for accuracy and trust
- AI-powered case summaries: Pre-populated insights that accelerate reviewer decision-making
- Automated medical record processing: Cutting down delays and admin burden
- Configurable workflows: Tailored to client-specific needs, with transparent outputs every step of the way
The Cohere Health difference in payment integrity
Our Payment Integrity Suite is designed to provide health plans with real flexibility and control:
- Insource payment integrity: Empower in-house teams with AI tools that drive accuracy and efficiency.
- Augment operations: Use automation to reduce administrative burden, institutionalize knowledge, and increase throughput.
- Delegate services: Partner with an AI-native vendor offering transparent processes and high-performing outcomes.
This approach allows health plans to move away from legacy models, reclaim control, and improve provider relationships in payment integrity while ensuring sustainable payment accuracy.
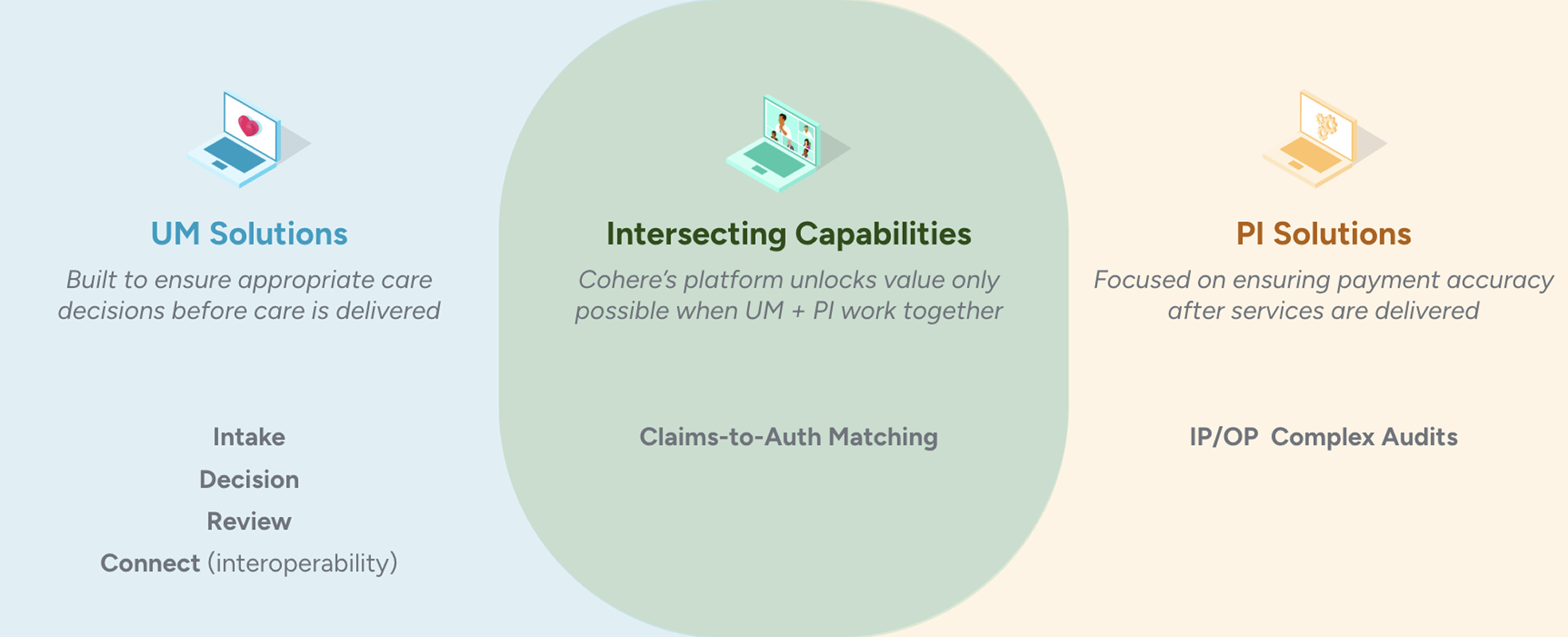
Looking ahead: Bridging UM and PI
The launch of Cohere Validate marks a milestone for Cohere Health’s clinical intelligence platform. With the recent acquisition of ZignaAI, we’re accelerating innovation in AI-powered payment integrity, bringing newfound transparency, efficiency, and control to health plans.
Our Payment Integrity Suite is already delivering measurable results—30% efficiency gains, 8–9x ROI, and faster payments- strengthening provider relationships in payment integrity. By unifying pre-service authorization data with post-service coding and clinical validation, Cohere creates a transparent ecosystem that reduces waste, improves collaboration, and ensures providers are paid promptly and accurately.
In addition to Cohere Validate, our broader PI Suite also includes:
- Cohere Match™ – a proprietary claims-to-authorization reconciliation solution to identify mismatches early and enable shift-left pre-pay claims strategies.
- Cohere Complete™ for PI – a modern services model that replaces legacy vendors with transparency, AI-powered efficiency, and lower contingency fees.
By combining clinical intelligence, AI automation, and flexible engagement models, we’re helping health plans move beyond opaque reviews toward configurable PI solutions that improve payment accuracy, provider trust, and overall healthcare economics.
Cohere Health will continue to innovate across the spectrum of pre-pay reviews and post-pay audits, enabling health plans to modernize their operations and improve the cost of care, payer-provider partnerships, and patient outcomes.
Cohere Validate is live as of September 9, 2025. Learn more about how our AI-powered payment integrity solutions can modernize your PI strategy at coherehealth.com/payment-integrity.
Available For Download
Written by

Cohere
Health
Cohere Health’s clinical intelligence platform delivers AI-powered solutions that streamline access to quality care by improving collaboration between physicians and health plans. Cohere works with 660,000 providers and processes millions of prior authorization requests annually. Its AI auto-approves up to 90% of requests for millions of health plan members. Cohere has been recognized in the Gartner® Hype Cycle™ for U.S. Healthcare Payers in 2024 and 2025, named a Top 5 LinkedIn™ Startup in 2023 and 2024, and is a three-time KLAS Points of Light award recipient.
Stay ahead with expert insights on transforming utilization management and payment integrity—delivered straight to your inbox.



