The hidden cost of prior authorization: Provider survey results
Published:
October 14, 2025

Prior authorization was designed to ensure appropriate use of medical services. It became one of healthcare's most frustrating bottlenecks—challenging providers and payers, delaying care, and creating administrative chaos that benefits no one.
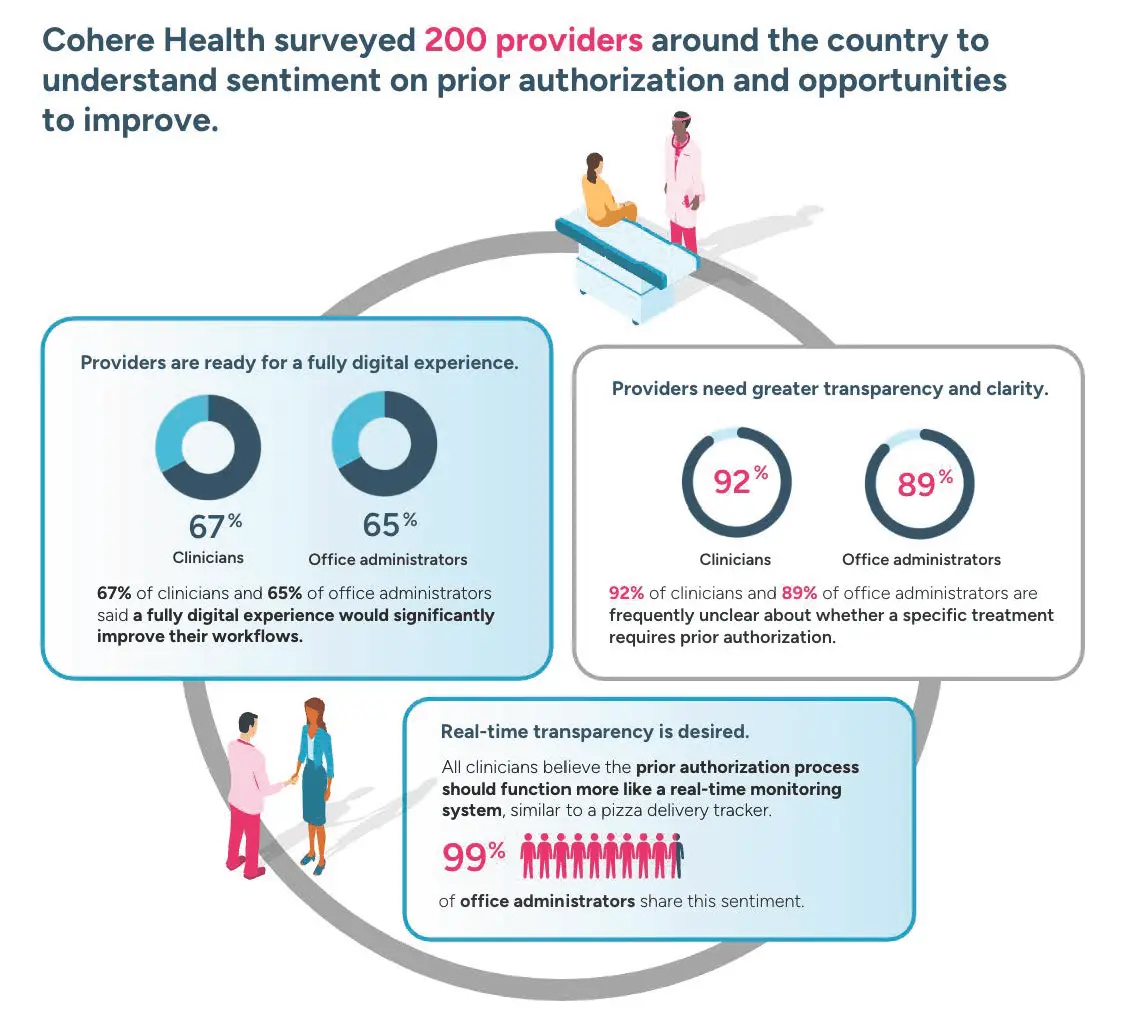
To better understand the problem, Cohere Health surveyed 200 clinicians and office professionals involved with prior authorization. Some of the findings you’d expect, and others are surprising.
Dangers of delays
The numbers tell a sobering story. Most providers have witnessed prior authorization delays leading to avoidable hospitalizations or emergency care. This isn't just an administrative annoyance—it's a patient safety issue hiding in plain sight. Ninety-seven percent of office administrators and 93% of clinicians report seeing prior authorization delays result in avoidable hospitalizations or emergency room visits.
The root cause? Unacceptable wait times for decisions. For clinicians and office administrators, delayed responses from health plans topped the list of biggest challenges. Currently, only 12% of clinicians and 7% of administrators report consistently receiving decisions within the federal timelines that will become mandatory on January 1, 2026: 72 hours for urgent cases and seven calendar days for standard requests.
The transparency challenge
Beyond delays, providers face a fundamental problem: they often don't know what they don't know. Ninety-two percent of clinicians and 89% of office administrators say they're frequently unclear about whether a specific treatment requires prior authorization from a health plan. For more than one in ten providers, this confusion is constant.
This uncertainty creates a cascade of problems. Providers waste time submitting unnecessary requests or, worse, delay care while trying to determine requirements. When requests are denied, providers often wait even longer to understand why—is it a submission issue, a coverage problem, or something else entirely? Until that's clear, the following steps remain stalled.
Inconsistent requirements across health plans compound these challenges. What one insurer requires for a patient may differ dramatically from another, forcing providers to navigate a patchwork of rules that change depending on which health plan and product their patient has.
The provider burden
Providers bear the administrative burden of the submission process. Ninety-two percent of clinicians and 95% of office administrators describe the prior authorization process as burdensome. For many, this manifests as daily workflow disruptions. Ten percent of both groups cite burnout as a direct result.
Providers also express frustration with a one-size-fits-all approach that doesn't reflect the realities of patient care. Sixty-five percent of clinicians and 55% of office administrators say the current process fails to account for the unique needs of different specialties, providers, or patients.
What providers want
The good news? Providers aren't resisting change—they're embracing it. Sixty-seven percent of clinicians and 65% of office administrators express a strong interest in a fully digital prior authorization experience. One hundred percent of clinicians and 99% of office administrators want real-time tracking capabilities to see where requests stand and when to expect decisions.
There's also remarkable openness to using AI. Ninety-nine percent of clinicians and 96% of office administrators trust AI to assist with prior authorization approvals. Forty-two percent of clinicians identify AI's most valuable role as pinpointing the right clinical documentation for submissions.
Providers also want consistency across health plans, integration with EHR systems, automated prompts for plan-specific requirements, and better communication channels with payers. These aren't pie-in-the-sky requests—they're practical solutions using existing technology.
The path forward
Federal mandates for faster turnaround times take effect January 1, 2026, creating both a deadline and an opportunity. Providers have spoken clearly about what they need: faster decisions, more transparency, and smarter technology to reduce the burden.
At Cohere Health, we’re helping health plans act on these insights, delivering AI-powered, digitally native prior authorization solutions that empower providers, improve member outcomes, and keep ahead of regulatory change.
Read more about Cohere Health’s provider survey results here.
Available For Download
Stay ahead with expert insights on transforming utilization management and payment integrity—delivered straight to your inbox.